Remote temperature monitoring to reduce the spread of COVID-19
Dr Charlotte JW Connell, School of Medicine; Dr Mike Laverick, Centre for eResearch
Research Team: Associate Professor Nicholas Gant, Department of Exercise Sciences; Professor Ralph Maddison, School of Population Health; Dr Charlotte Connell, School of Medicine; Hayden Green, Department of Exercise Sciences; Associate Professor Toby Mundel, School of Sport, Exercise and Nutrition, Massey University)

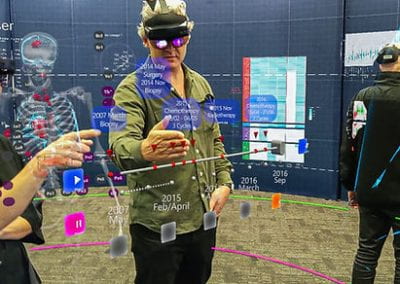
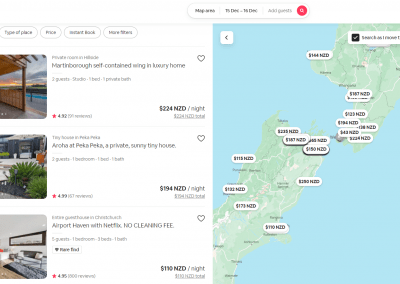
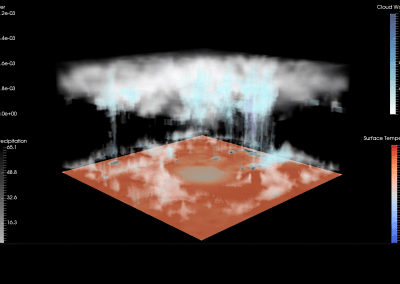
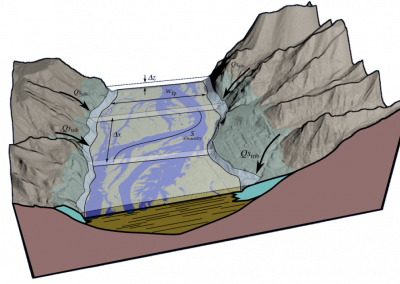
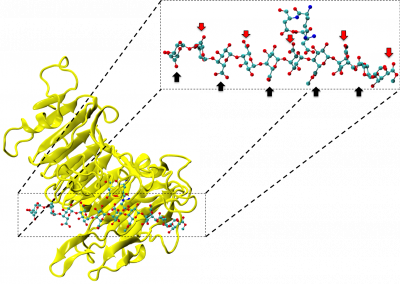
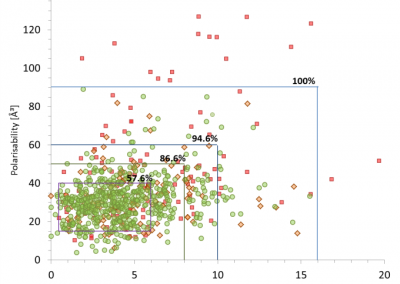
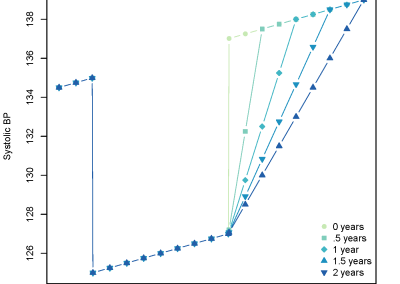
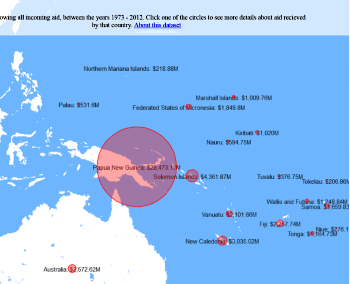
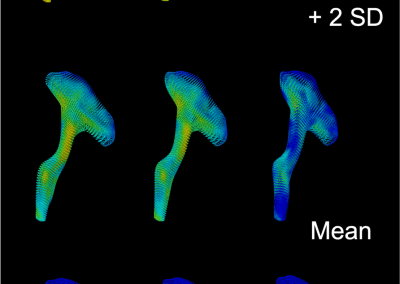
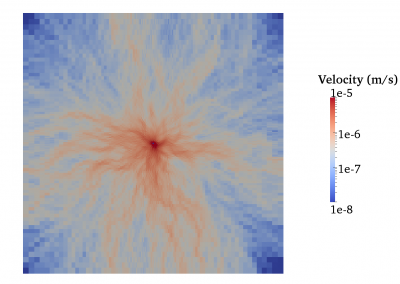
Figure 1. Clinical trials: data collected from Nightingale biosensor and synced with the mobile app.
Background
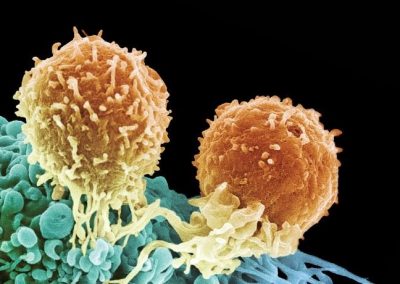
Elevated body temperature is an early clinical feature in around 90% of all COVID-19 cases, and a reduction in body temperature to normal levels is a key marker of recovery from the disease. Fever identification is an important tool for identifying possible infection from COVID-19 in lieu of diagnostic testing, and regular monitoring of body temperature can help catch COVID-19 cases early and prevent cluster outbreaks. Existing methods for monitoring measuring body temperature require healthcare personnel to make regular contact with people who may be infectious, increasing the risk of horizontal disease transmission. One promising approach to mitigate this risk involves using a new technology that consists of a small, matchbox-sized biosensor (called Nightingale, Figure 2) worn under the arm, within an insulated armband, capable of transmitting temperature data long-range directly to frontline healthcare staff. This wearable technology has a battery life of up to six weeks and can provide continuous body temperature monitoring of large groups of patients remotely, and automatically detect the presence of a fever, therein removing the need for physical contact for temperature monitoring.
Associate Professor Nicholas Gant and his research team in the Department of Exercise Sciences have been studying the use of this novel remote temperature monitoring system. The technology was invented in response to the COVID-19 global emergency, and its research and development has been funded by the Ministry of Business, Innovation and Employment (MBIE) COVID-19 Innovation Fund.
Methods and the role of the Centre for eResearch
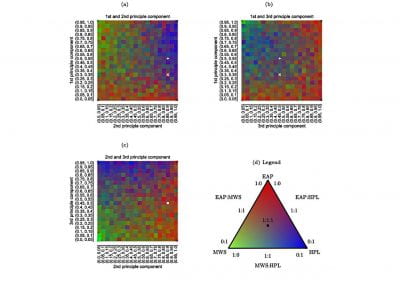
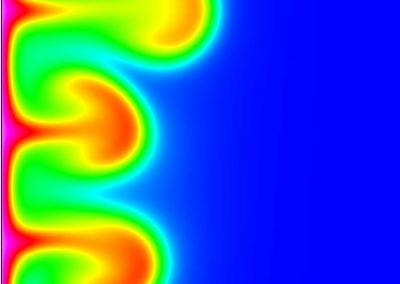
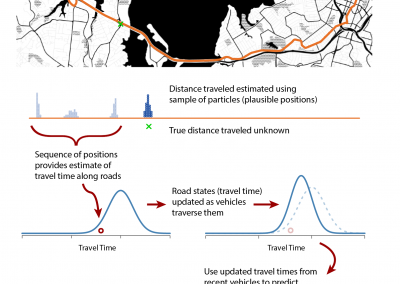
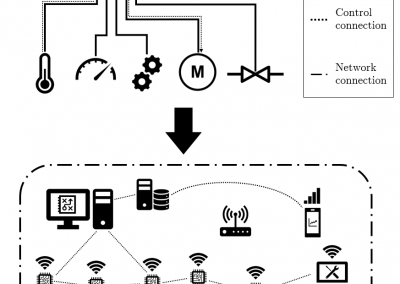
With the assistance of the Centre for eResearch, Gant and his research team have been able to push the trial data (Figure 1) collected on the devices to a secure virtual machine within the Nectar research cloud, which they have then used to run additional analyses and develop the algorithms that the armbands use to detect the presence of a fever.
In the first phase of the project, the body temperatures collected by the new device were compared against the most accurate methods of measuring core body temperature, such as rectal and gastrointestinal temperature. Although the armpit is one of the most hygienic and convenient places to measure body temperature, this site is not often used because the patient must keep their arm motionless for some time in order to get an accurate reading. Using laboratory tests, the team determined that the new device, through its continual wear, was capable of overcoming the limitations of traditional armpit temperature measurement, and collected enough viable data across a 24 hour period to be able to detect important changes in core body temperature. By using the Nectar research cloud the team were able to test the logistics and scalability of the remote-sensor data collection process.
Now the team will move into the second phase of the project, which involves testing the device in the real world-contexts that it is designed for. The device will be offered to clients staying in Managed Isolation Quarantine facilities, run by the New Zealand Government, and the temperature monitoring system will be used by healthcare staff working within these facilities, alongside their usual care. The armband will also be tested in several aged care facilities in the Auckland area, in order to examine the usability of the system for monitoring of vulnerable members of the community.

Figure 2. Matchbox-sized biosensor (called Nightingale).
Image from UoA news – https://www.auckland.ac.nz/en/news/2020/05/07/remote-temperature-device-for-rest-homes-a-world-first.html
See more case study projects

Our Voices: using innovative techniques to collect, analyse and amplify the lived experiences of young people in Aotearoa
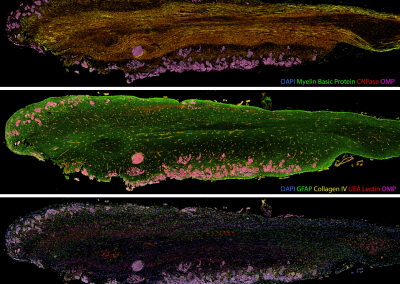
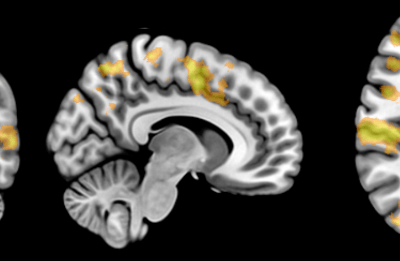
Painting the brain: multiplexed tissue labelling of human brain tissue to facilitate discoveries in neuroanatomy

Detecting anomalous matches in professional sports: a novel approach using advanced anomaly detection techniques

Benefits of linking routine medical records to the GUiNZ longitudinal birth cohort: Childhood injury predictors
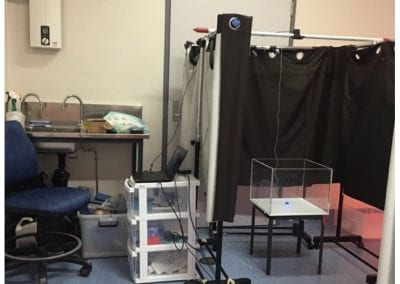
Using a virtual machine-based machine learning algorithm to obtain comprehensive behavioural information in an in vivo Alzheimer’s disease model
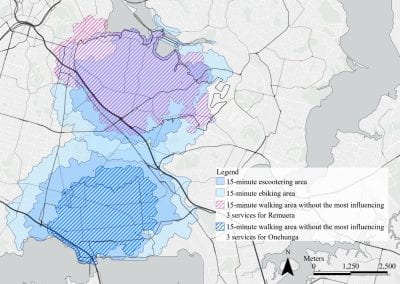
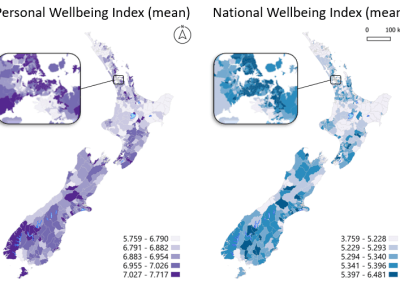
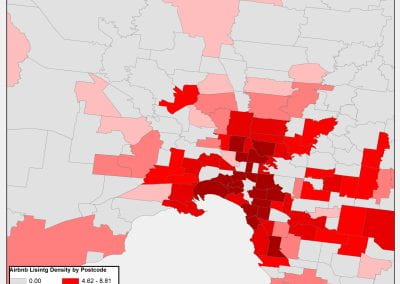
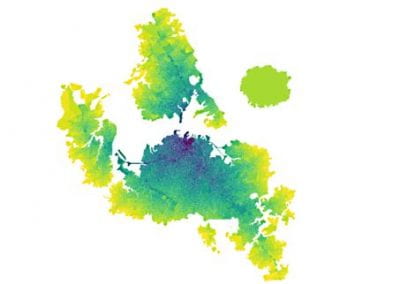
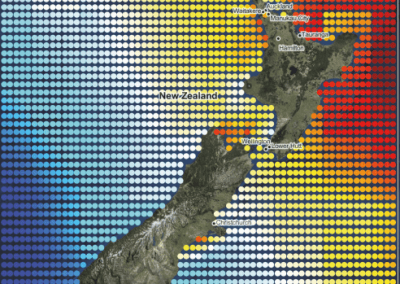
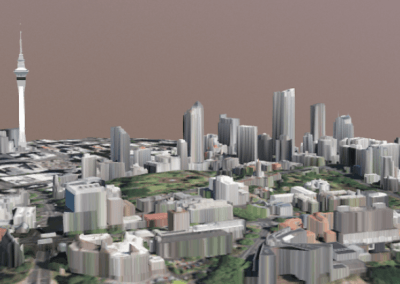
Mapping livability: the “15-minute city” concept for car-dependent districts in Auckland, New Zealand
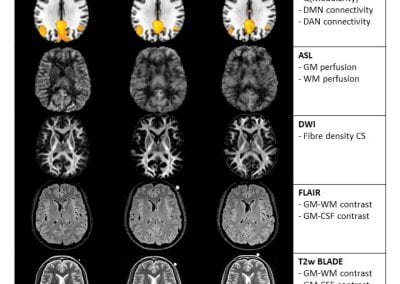
Travelling Heads – Measuring Reproducibility and Repeatability of Magnetic Resonance Imaging in Dementia
Novel Subject-Specific Method of Visualising Group Differences from Multiple DTI Metrics without Averaging

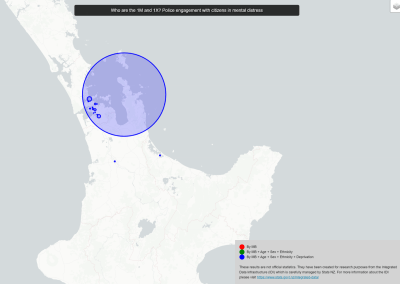
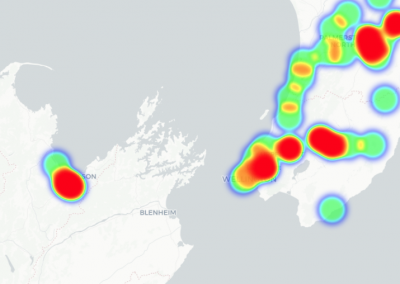
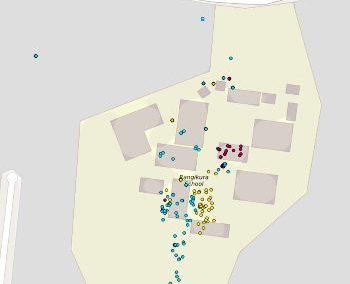
Re-assess urban spaces under COVID-19 impact: sensing Auckland social ‘hotspots’ with mobile location data

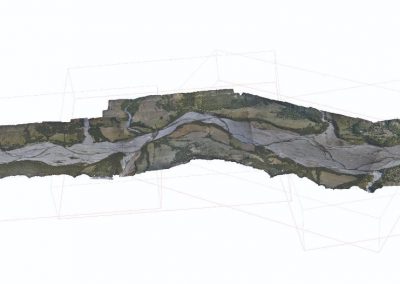
Aotearoa New Zealand’s changing coastline – Resilience to Nature’s Challenges (National Science Challenge)

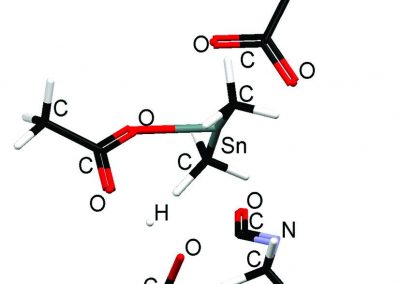
Proteins under a computational microscope: designing in-silico strategies to understand and develop molecular functionalities in Life Sciences and Engineering
Coastal image classification and nalysis based on convolutional neural betworks and pattern recognition
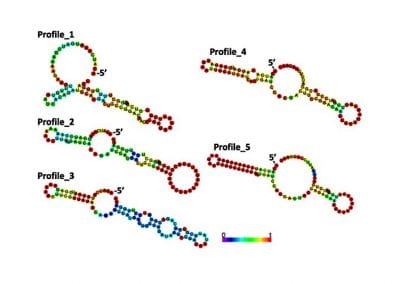
Determinants of translation efficiency in the evolutionarily-divergent protist Trichomonas vaginalis

Measuring impact of entrepreneurship activities on students’ mindset, capabilities and entrepreneurial intentions

Using Zebra Finch data and deep learning classification to identify individual bird calls from audio recordings
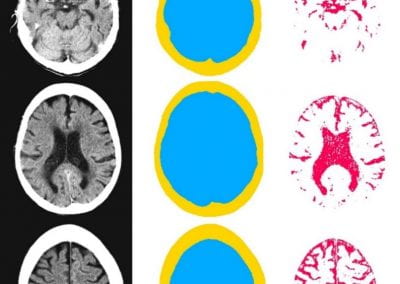
Automated measurement of intracranial cerebrospinal fluid volume and outcome after endovascular thrombectomy for ischemic stroke

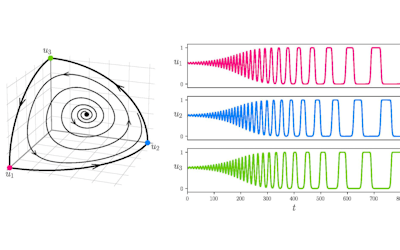
Using simple models to explore complex dynamics: A case study of macomona liliana (wedge-shell) and nutrient variations
Fully coupled thermo-hydro-mechanical modelling of permeability enhancement by the finite element method

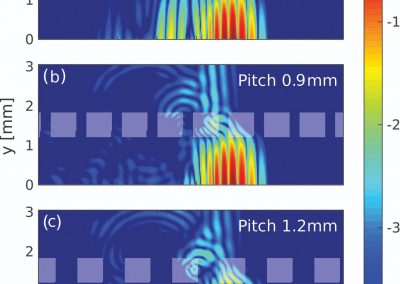
Modelling dual reflux pressure swing adsorption (DR-PSA) units for gas separation in natural gas processing
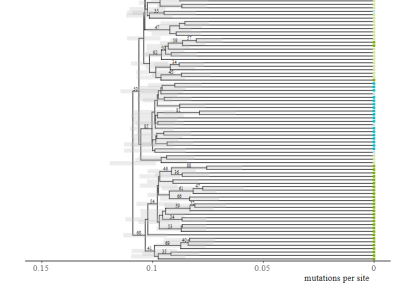
Molecular phylogenetics uses genetic data to reconstruct the evolutionary history of individuals, populations or species
Wandering around the molecular landscape: embracing virtual reality as a research showcasing outreach and teaching tool