Improving the treatment of heart disease
Susann Beier, Faculty of Medical and Health Sciences
Coronary artery disease is the most common killer in the Western world. One in four people will die from a blockage in one of the coronary arteries, preventing supply of blood and oxygen to the heart.
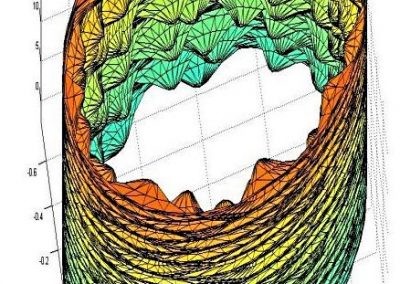
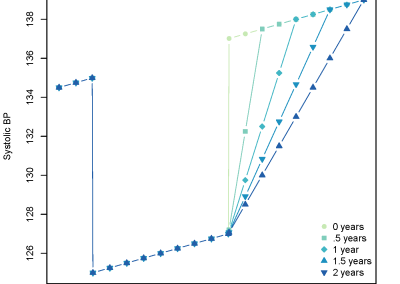
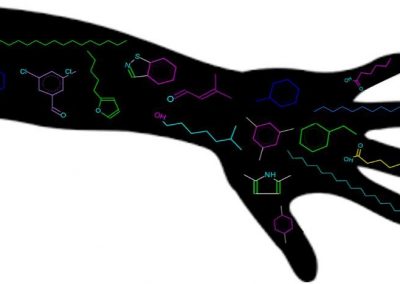
A common treatment for narrowed arteries is ‘Percutaneous Coronary Intervention’ or PCI, where a wire mesh tube, or ‘stent’, is inserted into the narrowed blood vessel and expanded to hold it open. The expansion of the stent compresses the abnormal build-up of atheroma narrowing the artery. This is a highly effective and relatively low risk treatment, it avoids surgery, and enables rapid improvement in the patient’s condition. Unfortunately, stents fail in 25% of patients, when the previous narrowing reoccurs within the stent. New stents which release medication (known as ‘drug-eluting’ stents) promised a solution to this problem, with the slow local release of drugs supressing the regrowth of the tissue responsible for re- narrowing. A short-term improvement is achieved, but late failure rates still carry the risk of causing sudden death.
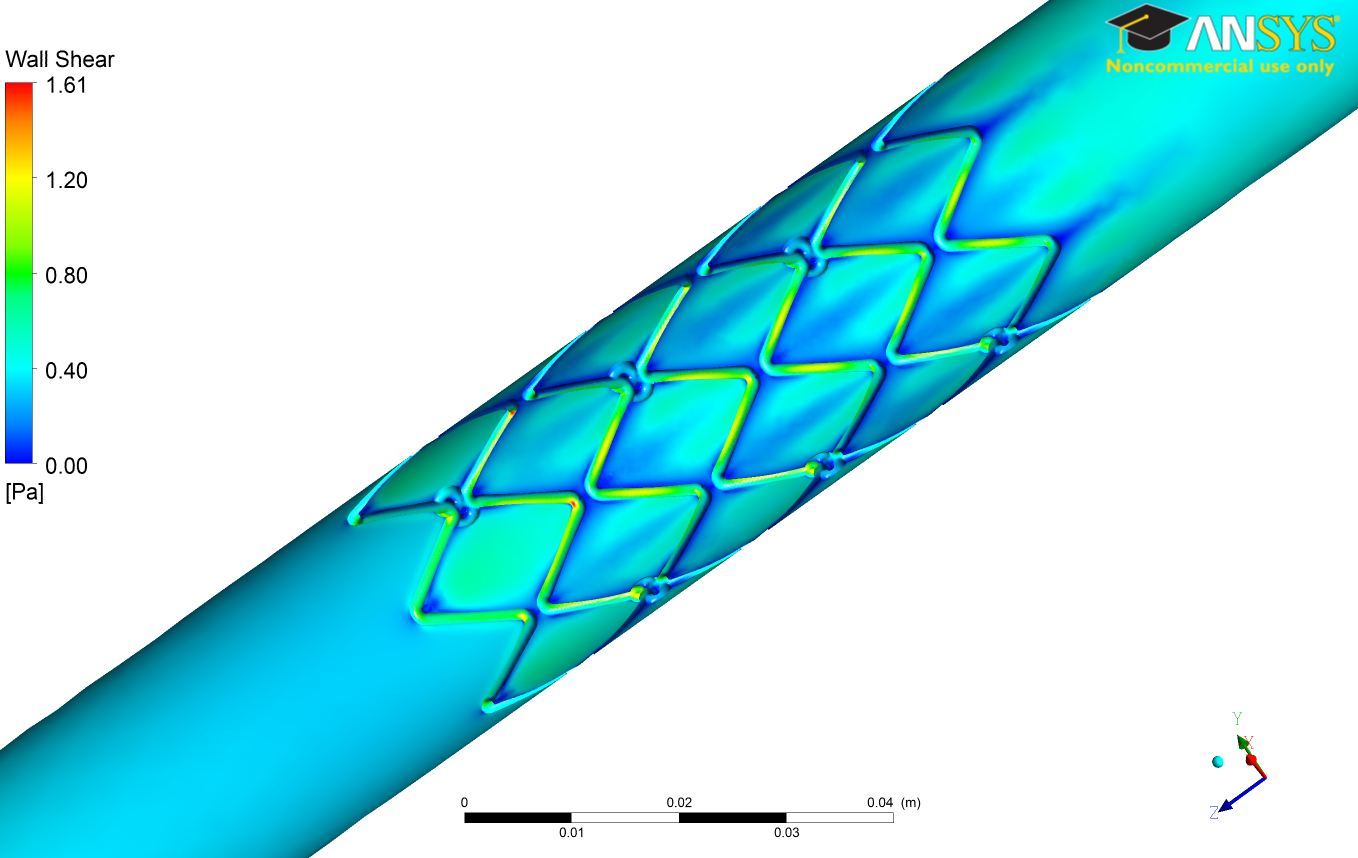
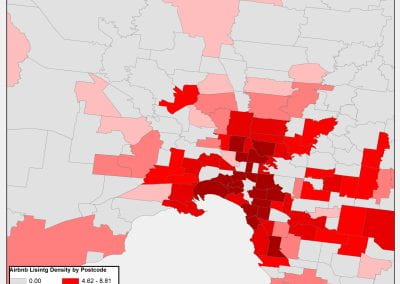
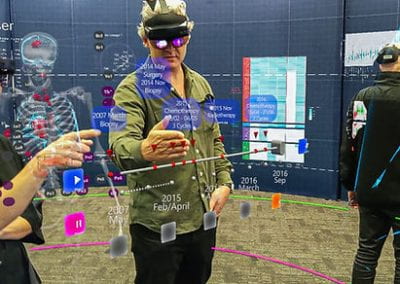
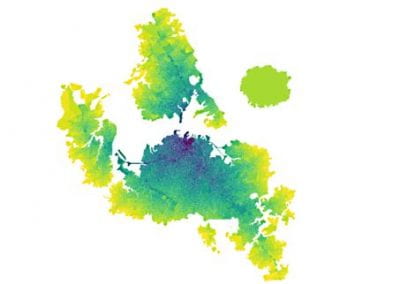
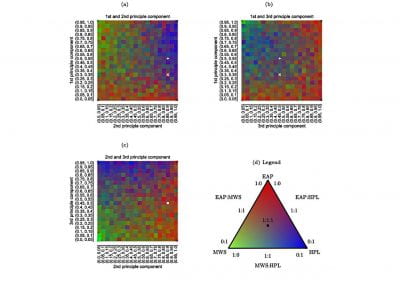
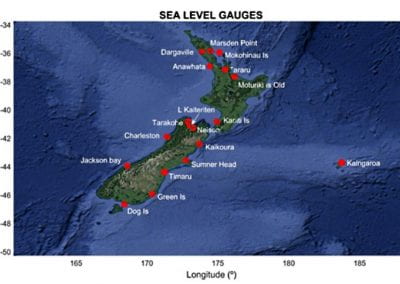
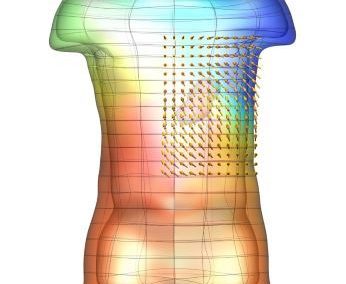
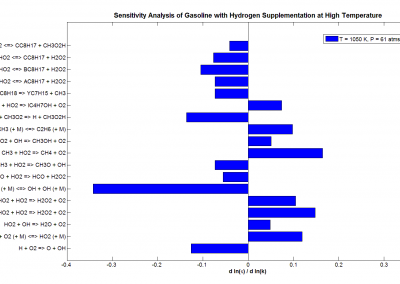
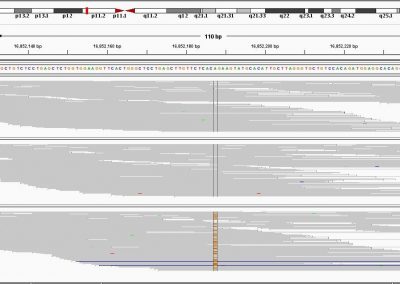
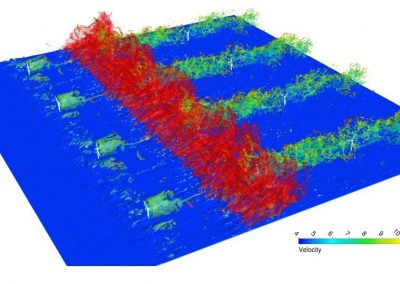
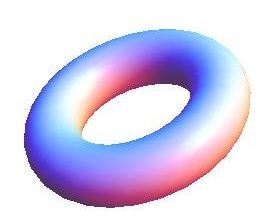
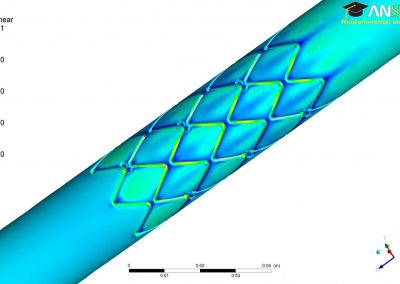
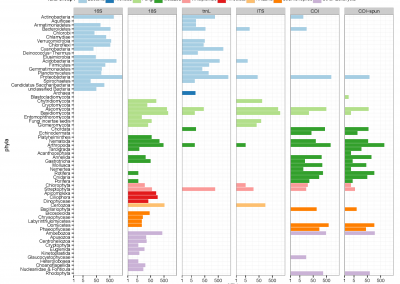
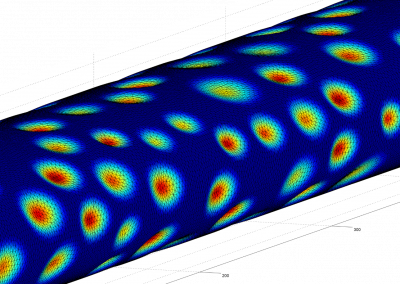
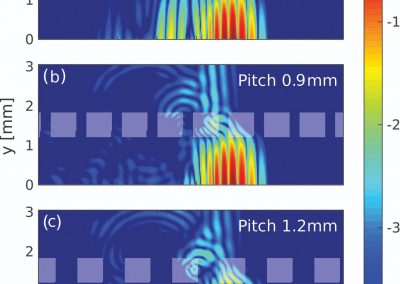
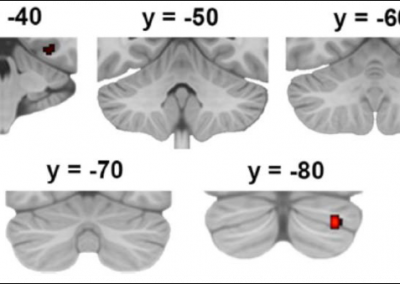
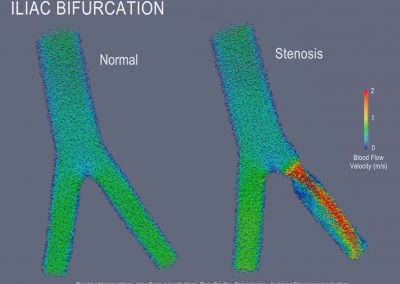
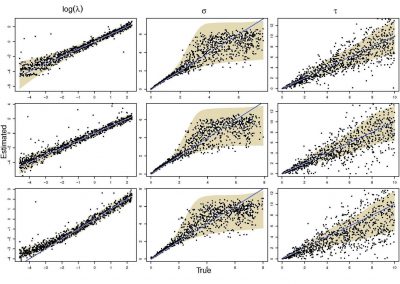
Figure 1: Stress in the wall of a coronary artery after stent implanted
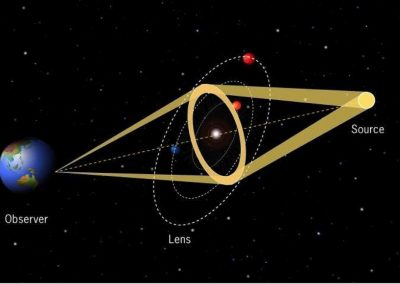
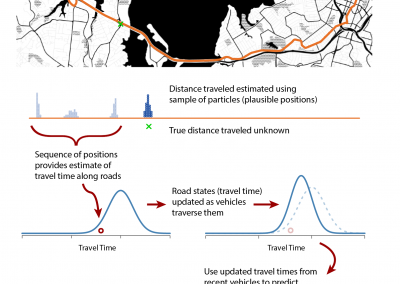
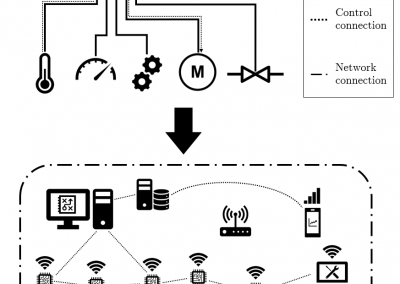
It is known that the presence of the stent changes blood flow, which in turn alters the growth of tissue, and thereby affects treatment outcome. Currently, there are more than 250 different stent designs available, each of which has a different effect on the 3D pattern of blood flow. The stent design is therefore critically important in determining treatment success or failure. Clinical trials with groups of patients have been unable to define the stent design features which determine success or failure due to the complexity of the problem. More detailed quantitative analysis is needed to answer the question of how different stent designs affect the complex blood flow through the coronary arteries.
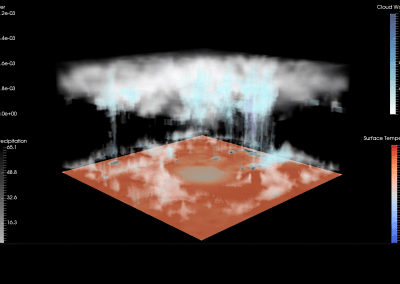
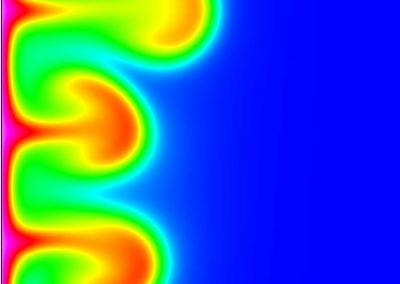
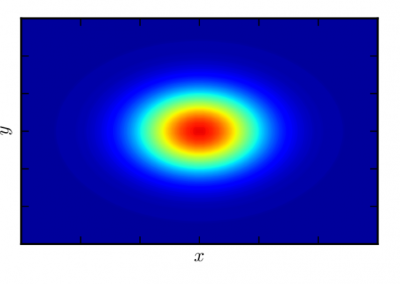
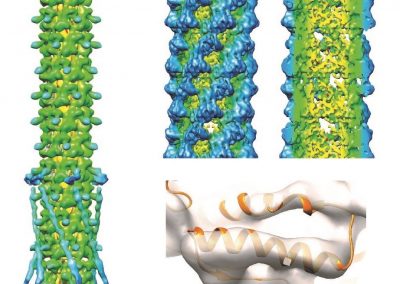
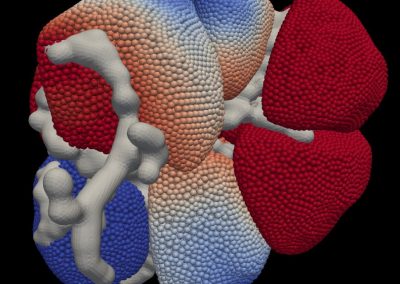
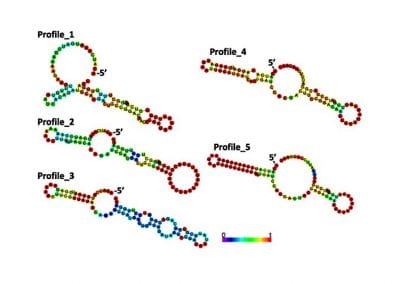
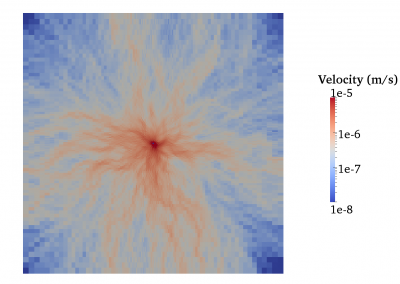
My research aims to study the link between stent design features, the changes they cause in blood flow (haemodynamics), and the impact on patient outcome. Computational Fluid Dynamic (CFD) modelling was used to quantify the haemodynamics for various stent designs. This allowed the calculation of blood velocity, the stress the blood flow induces on the vessel wall, and to detect regions of rapid changes by simulating the vessel shape, circulation and blood rheology. Two commonly used stent designs were modelled to determine their respective strengths and weaknesses.
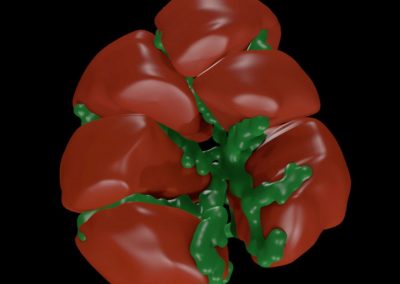
In addition to the computational simulations, a number of blood vessels were scaled up, manufactured in plastic using 3D printing and connected to a pump to simulate the heart. They were then placed in an MRI scanner to measure the blood flow with PC-MR (Phase-Contrast Magnetic Resonance). A comparison was then performed between the computational CFD and experimental MRI data with good agreement found.
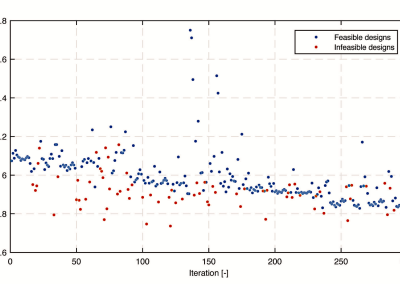
Simulating coronary blood flow on the Pan cluster
Many simulation time steps were required to accurately represent the rapidly changing flow conditions in the coronaries with more than 2,500 time steps computed for a single heartbeat. To ensure full development of the flow, four heartbeats were modelled, and only the last was analysed. Each simulation contained approximately 20 million elements, and used multi-threading over six cores with 40CPUs and with 20GB of memory each, and took around 48 hours to solve.
This task would have not been possible without the Pan cluster, as the memory requirements would have exceeded local desktop capabilities well before a possibly month long solution was obtained. We were able to run many simulations on the cluster, allowing us to systematically investigate more than 20 different stent design aspects, and their impact on blood flow in the coronary arteries.
Next steps
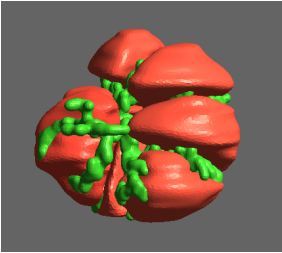
Due to the Pan cluster resource we are now extending our research to more complex vessel geometries such as vessel branching. Having gained a greater understanding of the features that are critical to idealised stent design, the next milestone is to model a stented coronary artery from an actual patient. This is a highly complex undertaking but the knowledge that can be gained will have an important impact in the treatment of patients with heart disease.
See more case study projects

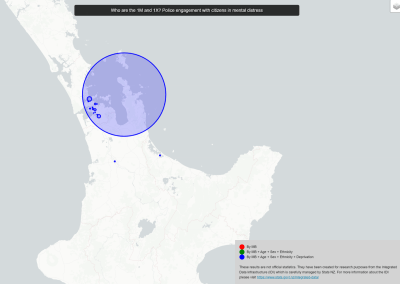
Our Voices: using innovative techniques to collect, analyse and amplify the lived experiences of young people in Aotearoa
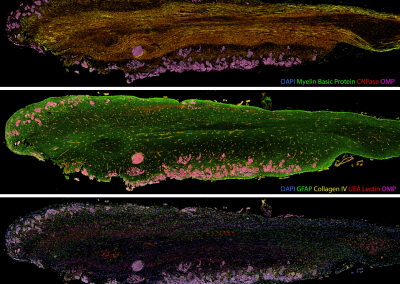
Painting the brain: multiplexed tissue labelling of human brain tissue to facilitate discoveries in neuroanatomy

Detecting anomalous matches in professional sports: a novel approach using advanced anomaly detection techniques

Benefits of linking routine medical records to the GUiNZ longitudinal birth cohort: Childhood injury predictors

Using a virtual machine-based machine learning algorithm to obtain comprehensive behavioural information in an in vivo Alzheimer’s disease model
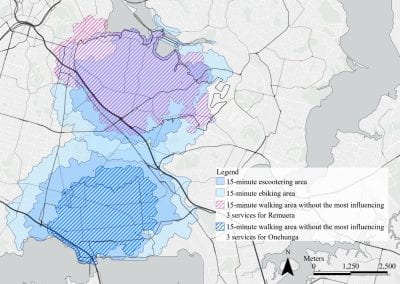
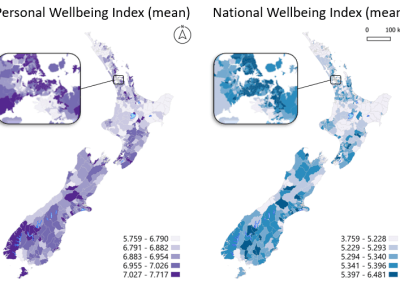
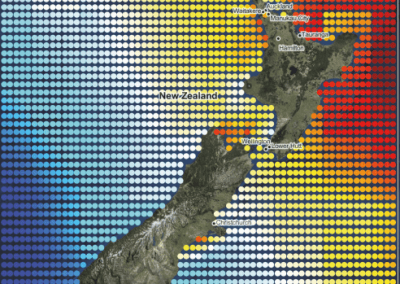
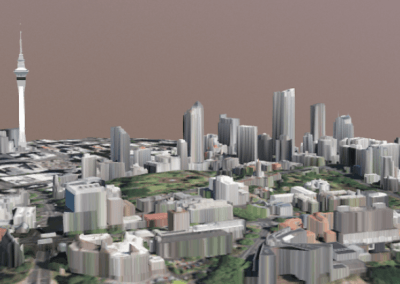
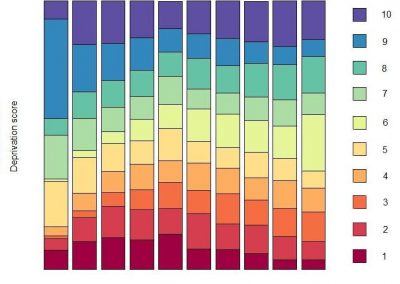
Mapping livability: the “15-minute city” concept for car-dependent districts in Auckland, New Zealand
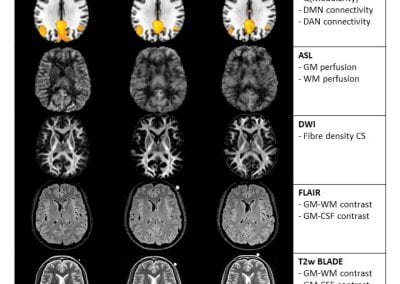
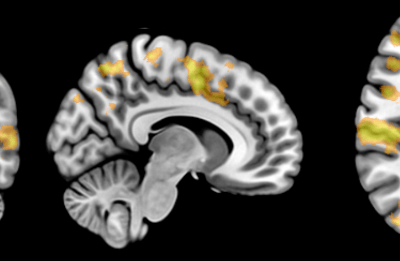
Travelling Heads – Measuring Reproducibility and Repeatability of Magnetic Resonance Imaging in Dementia
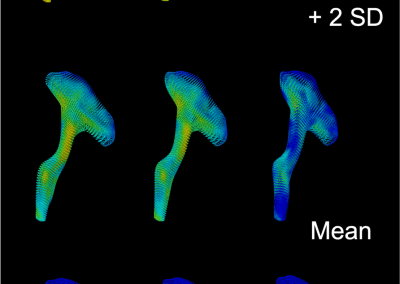
Novel Subject-Specific Method of Visualising Group Differences from Multiple DTI Metrics without Averaging

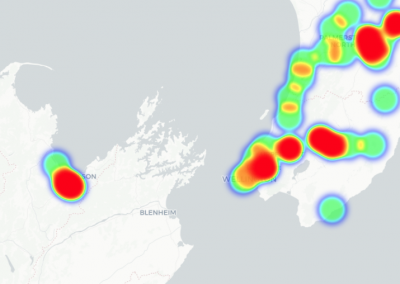
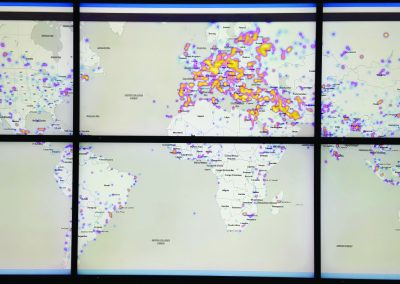
Re-assess urban spaces under COVID-19 impact: sensing Auckland social ‘hotspots’ with mobile location data

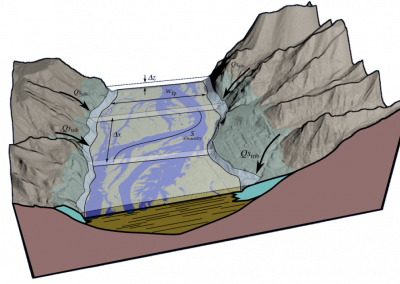
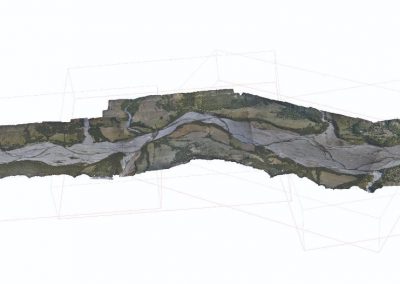
Aotearoa New Zealand’s changing coastline – Resilience to Nature’s Challenges (National Science Challenge)

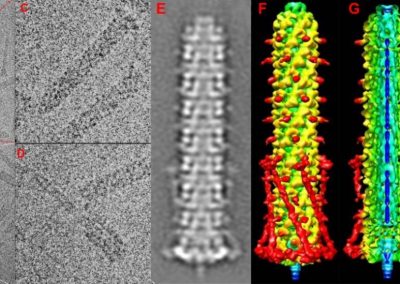
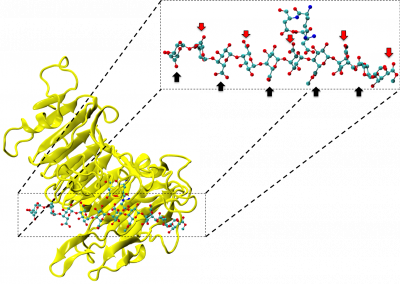
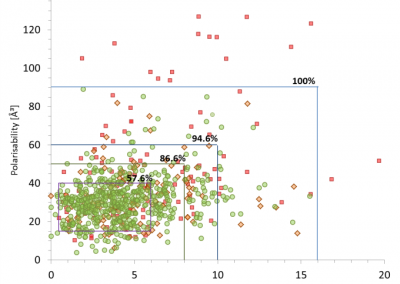
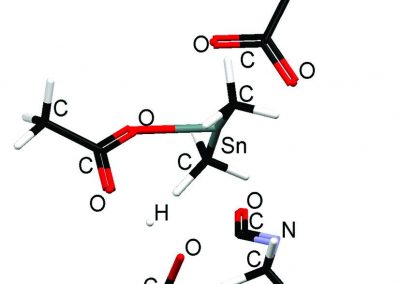
Proteins under a computational microscope: designing in-silico strategies to understand and develop molecular functionalities in Life Sciences and Engineering
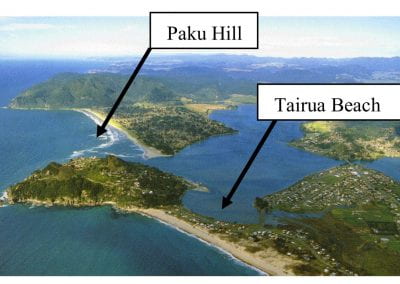
Coastal image classification and nalysis based on convolutional neural betworks and pattern recognition
Determinants of translation efficiency in the evolutionarily-divergent protist Trichomonas vaginalis
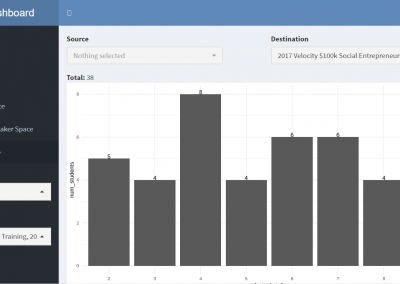
Measuring impact of entrepreneurship activities on students’ mindset, capabilities and entrepreneurial intentions

Using Zebra Finch data and deep learning classification to identify individual bird calls from audio recordings
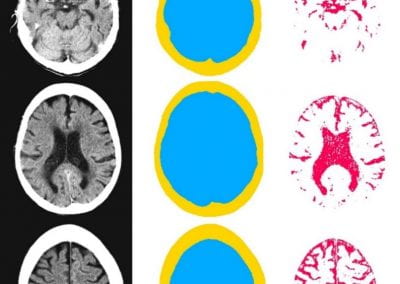
Automated measurement of intracranial cerebrospinal fluid volume and outcome after endovascular thrombectomy for ischemic stroke

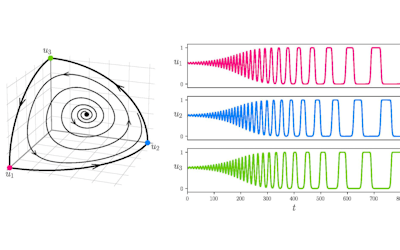
Using simple models to explore complex dynamics: A case study of macomona liliana (wedge-shell) and nutrient variations
Fully coupled thermo-hydro-mechanical modelling of permeability enhancement by the finite element method

Modelling dual reflux pressure swing adsorption (DR-PSA) units for gas separation in natural gas processing
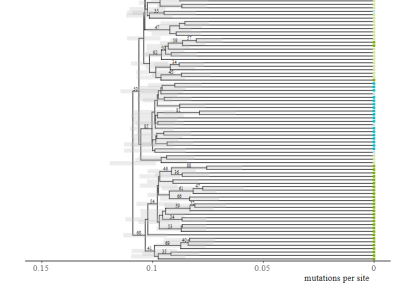
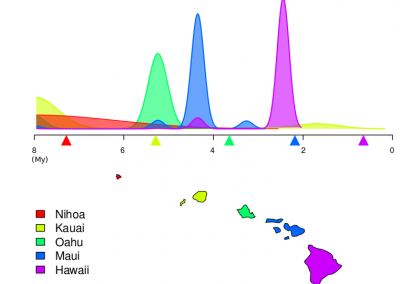
Molecular phylogenetics uses genetic data to reconstruct the evolutionary history of individuals, populations or species
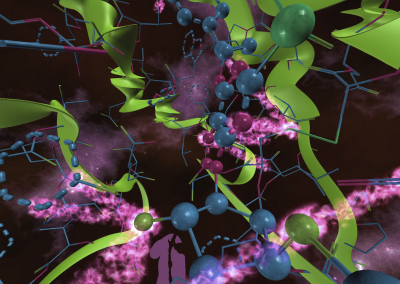
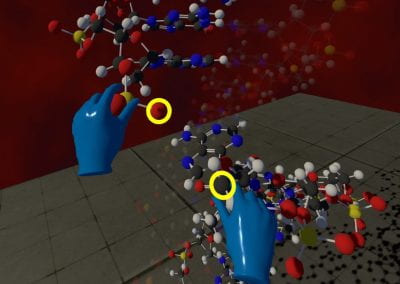
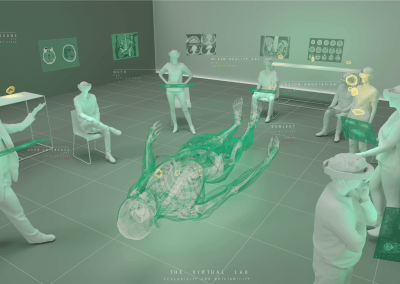
Wandering around the molecular landscape: embracing virtual reality as a research showcasing outreach and teaching tool