Quality of care and outcomes in children with cleft lip and/or palate
Louise Ayrey, Project Manager, PhD candidate, Department of Paediatrics – Child and Youth Health
Objectives
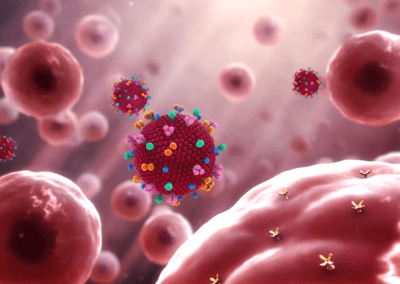
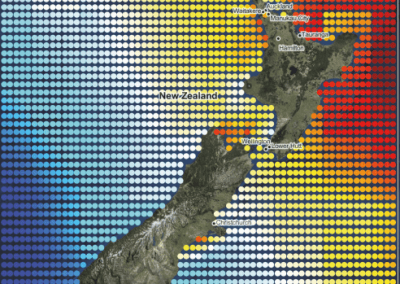
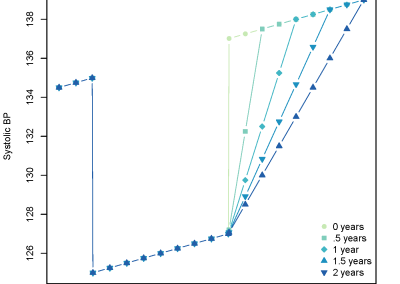
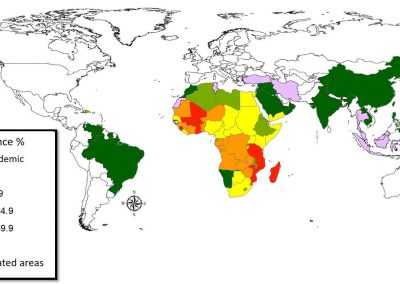
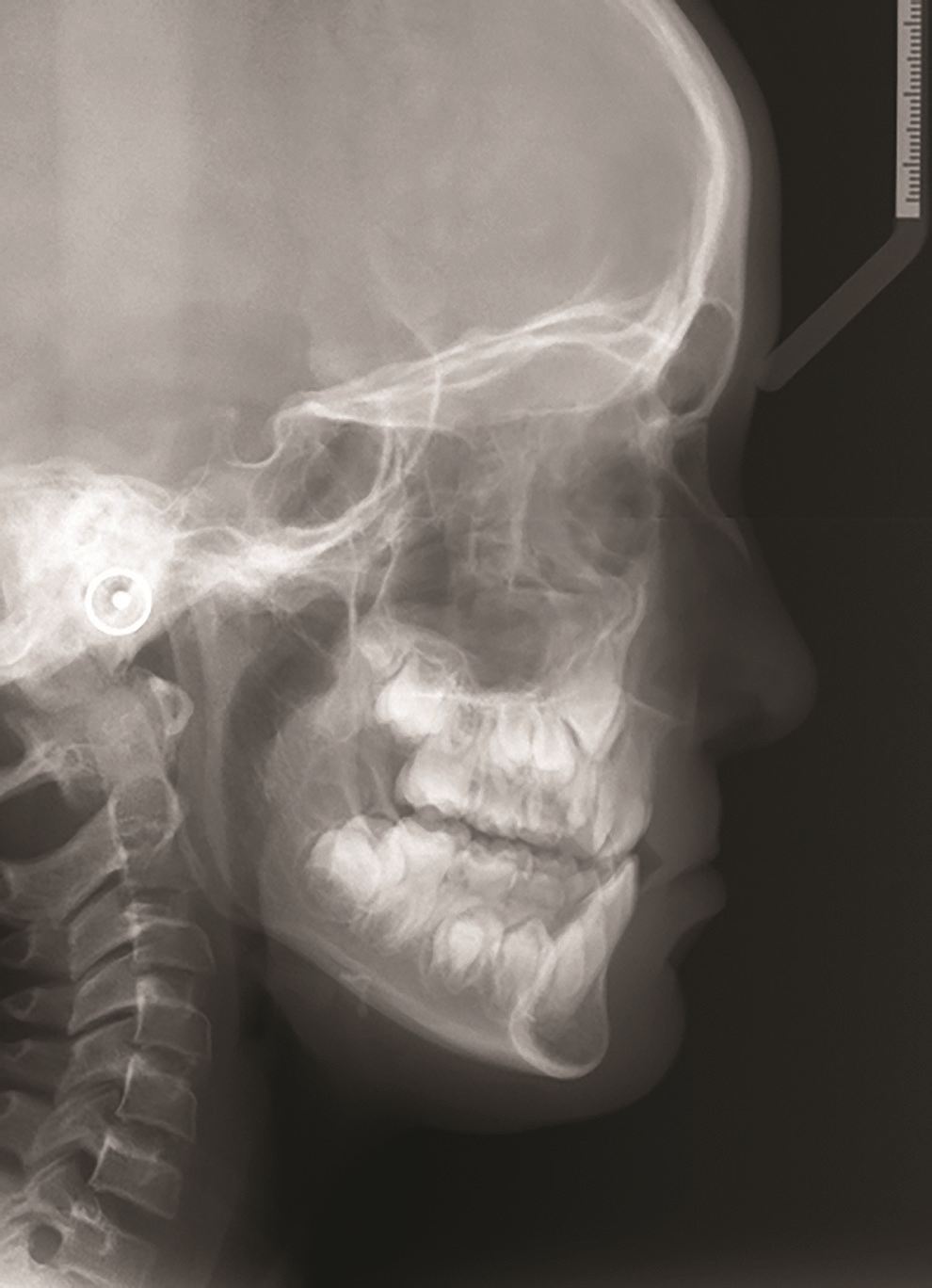
This study has two main objectives in relation to cleft lip and palate (CLP). Firstly it will investigate the health care delivery pathways from the time of diagnosis to the primary surgery for children with a cleft lip and/or palate and their families. This will ensure that CLP patients are receiving health delivery to the standard expected and required. Secondly it will provide the first consistently collected outcome data in relation to cleft lip and palate in New Zealand, including surgical outcomes, speech, dental care and importantly quality of life. This study will be compared to data from the UK to determine how cleft lip and palate patients in New Zealand fare compared to their contemporaries worldwide. This will allow any deficiencies to be identified and processes put in place to ensure improved outcomes in the future Cleft lip and/or palate (CLP) is a most common birth defect affecting approximately 1 in 700 newborn infants. In New Zealand we have found a higher incidence (1 in 566 live births). Of note was a higher rate of cleft palate alone in Maori (the highest reported in the world), followed by Pacific and others.
The treatment for those born with CLP is long term (usually till at least one’s early 20’s) and multidisciplinary (involving multiple surgeries, speech language therapy, and orthodontic treatment) as well as having an impact on quality of life of both the child and the family. There is little data relating to health delivery of cleft services in New Zealand and the outcomes associated with the delivery of these services.
This project has three main aims
- To determine the care paths and family satisfaction of pathways from diagnosis to primary surgery and ensure cleft services are being provided at the highest level.
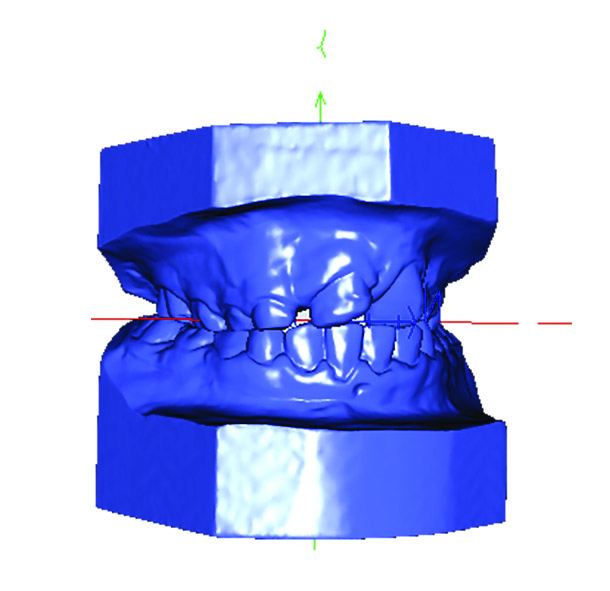
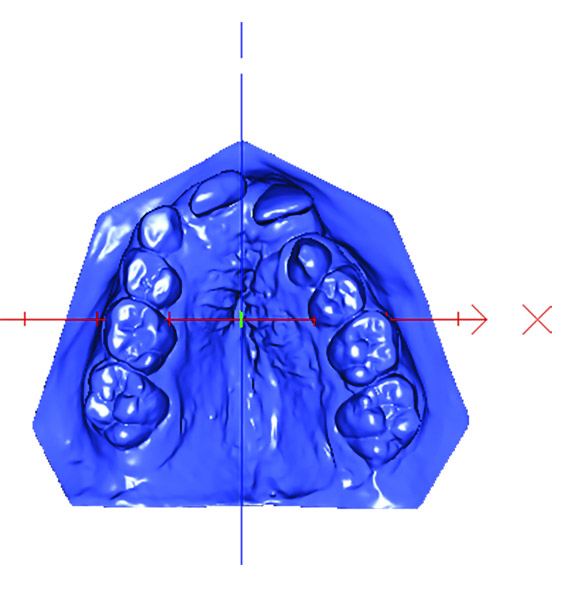
- To assess a range of clinical and personal outcomes in CLP patients at 5 and 8-10 years of age.
- To assess how outcomes for New Zealand CLP patients compare to those of CLP patients in Australia and the United Kingdom.
How are we doing this?
To ensure we meet the project’s aims the cooperation and collaboration of a number of health professionals is required. We are utilising staff within the cleft multidisciplinary teams to ensure the timely and accurate collection and reporting of speech, orthodontic, photographic, growth and quality of life data. Dental health data is also being collected from 20 DHB’s.
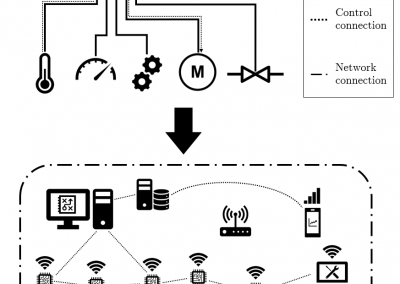
Using the university’s research VM to upload and keeping data safe with Seafile
With numerous people uploading data from several hospitals across a number of locations in a timely manner, it was imperative a secure, safe portal was established from the outset. The Centre for eResearch support team has provided an encrypted secure mechanism for file sharing and storage services using open source Seafile software installed in the university’s research virtual machines (RVM). This enables the upload of patient data with secure password protection for each user and the added protection of passwords within each sub-section of the study. Principal investigators can quickly assess how much of each data set is coming in, when it was uploaded and from whom. Assigning study ID and renaming files shortly after they arrive into the database enhances the speed at which we can ensure the study subjects remain unidentified for assessment purposes. The subsequent downloading of the de-identified data from Seafile to be used by the investigators for scoring and analysis is also fast and efficient.
Where to in the future?
This project aligns with the goals set out for the Health Delivery stream. It will be able to deliver robust information about pathways and outcomes that will enable changes to policy and practice to ensure consistency and best outcomes for CLP patients in New Zealand within 5 years. This research will impact on the delivery of cleft services in New Zealand and help to optimise appropriate standardised care pathways after antenatal diagnosis of a pregnancy with a cleft (through the Maternal=Fetal Medicine network). Early life data will enable health services to plan suitable health care for cleft children (via the newborn network). The outcomes will enable establishment of baseline data for New Zealand as well as providing detailed data on factors affecting outcomes in cleft children throughout childhood. It will also provide evidence of how New Zealand units are faring relative to our Australian counterparts as well as established best practice units in the United Kingdom.
See more case study projects

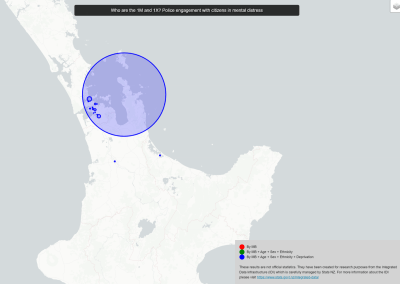
Our Voices: using innovative techniques to collect, analyse and amplify the lived experiences of young people in Aotearoa
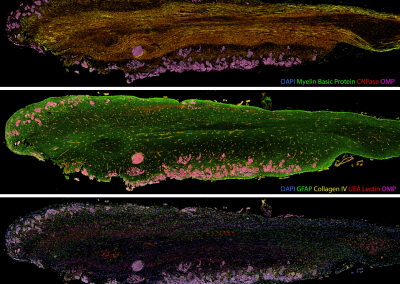
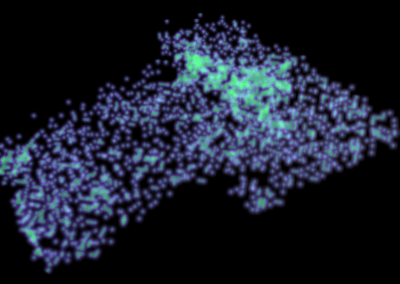
Painting the brain: multiplexed tissue labelling of human brain tissue to facilitate discoveries in neuroanatomy

Detecting anomalous matches in professional sports: a novel approach using advanced anomaly detection techniques

Benefits of linking routine medical records to the GUiNZ longitudinal birth cohort: Childhood injury predictors
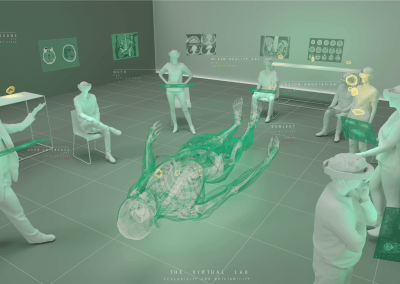
Using a virtual machine-based machine learning algorithm to obtain comprehensive behavioural information in an in vivo Alzheimer’s disease model
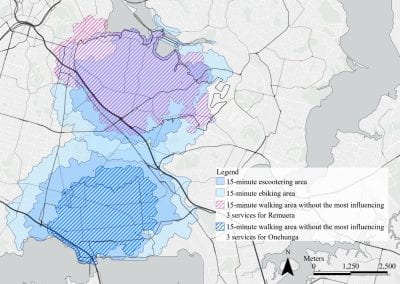
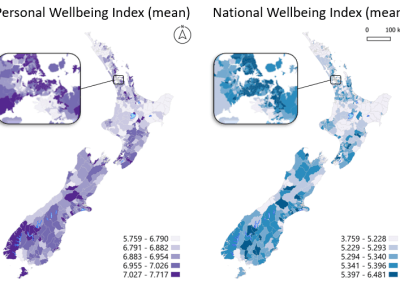
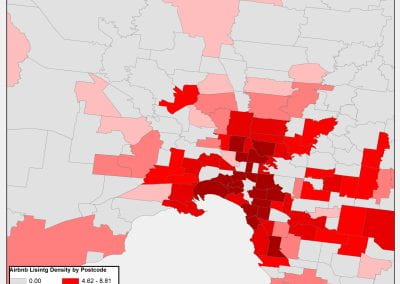
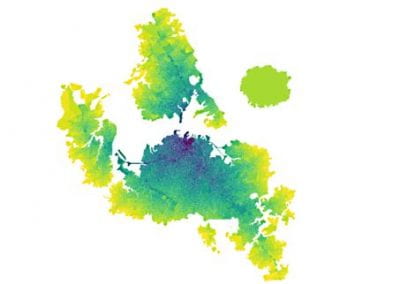
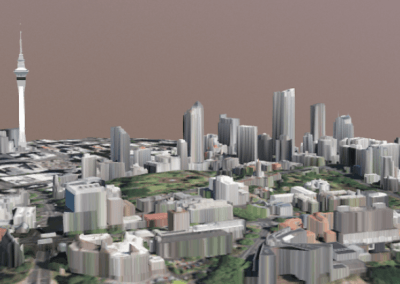
Mapping livability: the “15-minute city” concept for car-dependent districts in Auckland, New Zealand
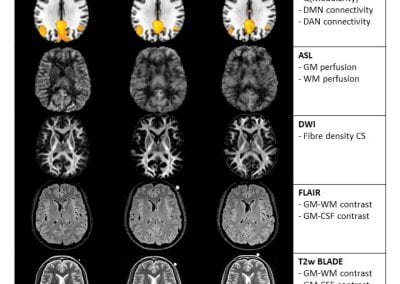
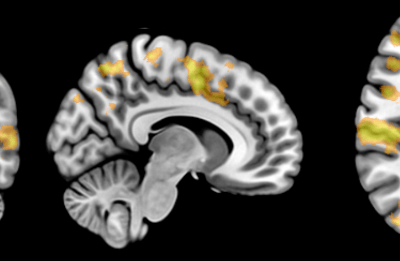
Travelling Heads – Measuring Reproducibility and Repeatability of Magnetic Resonance Imaging in Dementia
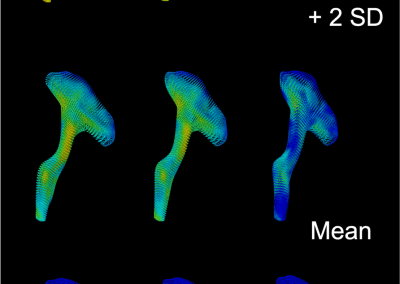
Novel Subject-Specific Method of Visualising Group Differences from Multiple DTI Metrics without Averaging

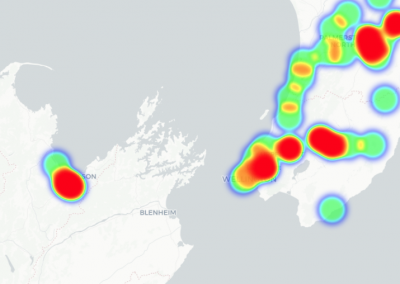
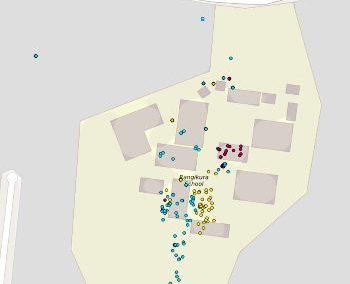
Re-assess urban spaces under COVID-19 impact: sensing Auckland social ‘hotspots’ with mobile location data

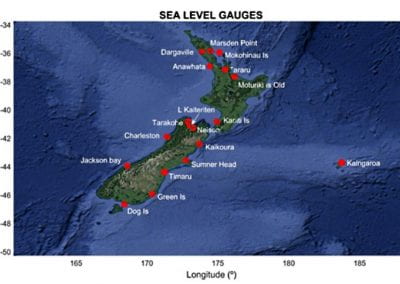
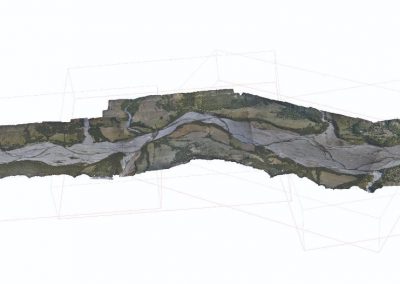
Aotearoa New Zealand’s changing coastline – Resilience to Nature’s Challenges (National Science Challenge)

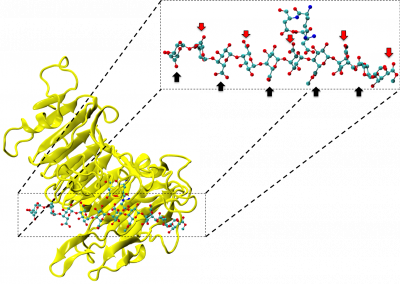
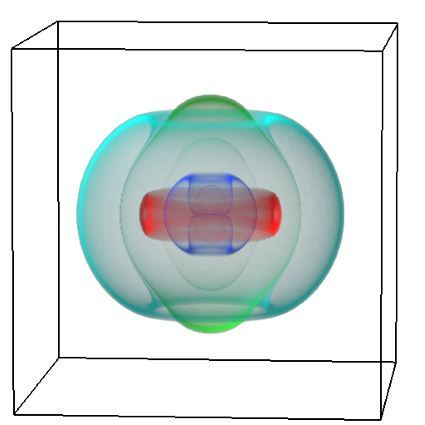
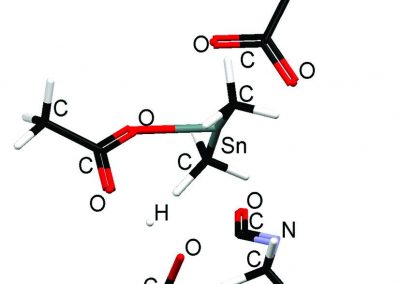
Proteins under a computational microscope: designing in-silico strategies to understand and develop molecular functionalities in Life Sciences and Engineering
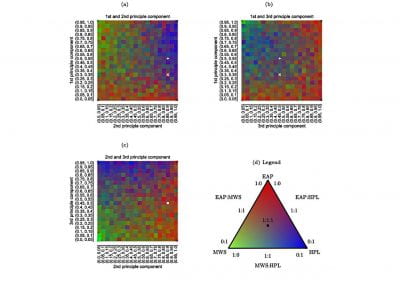
Coastal image classification and nalysis based on convolutional neural betworks and pattern recognition
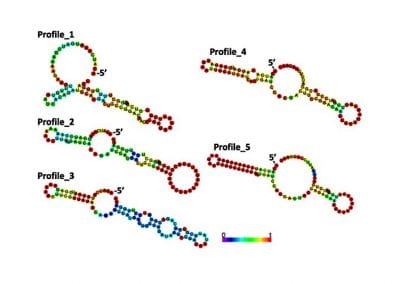
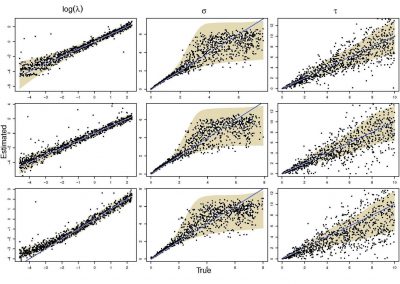
Determinants of translation efficiency in the evolutionarily-divergent protist Trichomonas vaginalis

Measuring impact of entrepreneurship activities on students’ mindset, capabilities and entrepreneurial intentions

Using Zebra Finch data and deep learning classification to identify individual bird calls from audio recordings
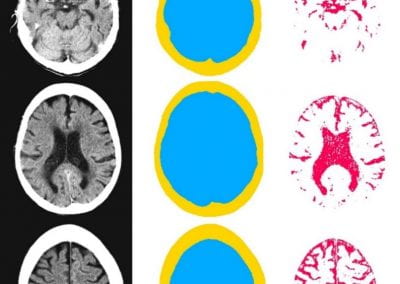
Automated measurement of intracranial cerebrospinal fluid volume and outcome after endovascular thrombectomy for ischemic stroke

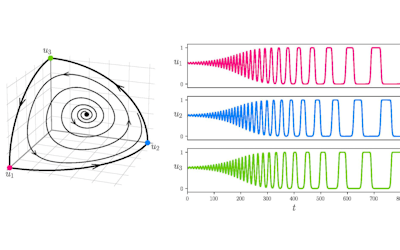
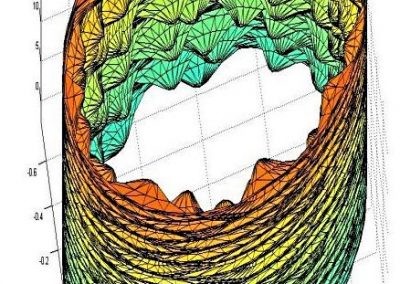
Using simple models to explore complex dynamics: A case study of macomona liliana (wedge-shell) and nutrient variations
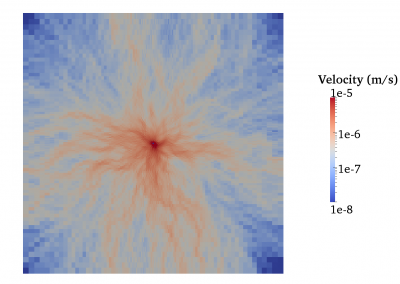
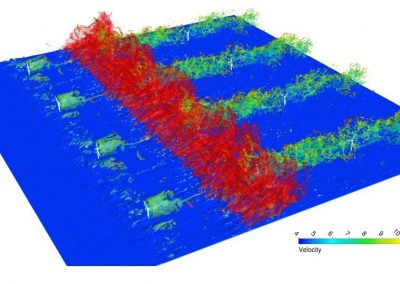
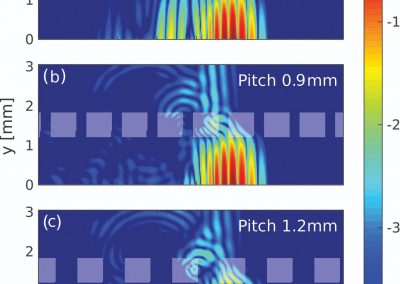
Fully coupled thermo-hydro-mechanical modelling of permeability enhancement by the finite element method

Modelling dual reflux pressure swing adsorption (DR-PSA) units for gas separation in natural gas processing
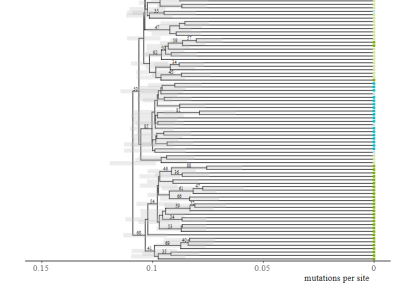
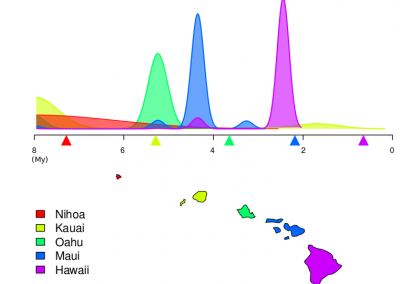
Molecular phylogenetics uses genetic data to reconstruct the evolutionary history of individuals, populations or species
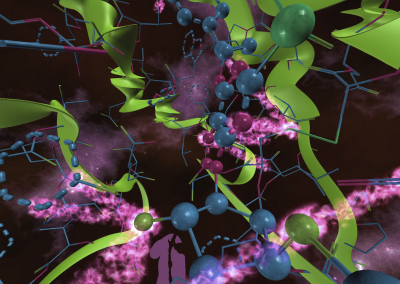
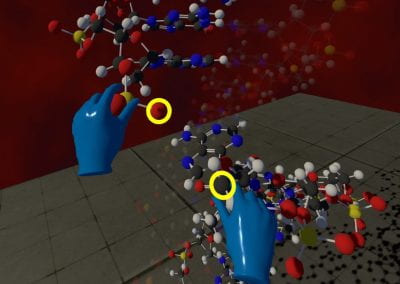
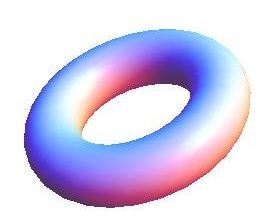
Wandering around the molecular landscape: embracing virtual reality as a research showcasing outreach and teaching tool